Amniocentesis
Amniocentesis or amniotic fluid test is an invasive prenatal diagnostic examination in which a sample of amniotic fluid is taken from the amniotic sac that surrounds the baby. The purpose of this procedure is to discover possible chromosomal, genetic or metabolic diseases of your baby before birth.
- Who will benefit from the amniocentesis?
- What chromosomal and genetic tests can be carried out with the amniotic fluid taken during amniocentesis?
- What do incidental findings during the NGS analysis mean and why it is necessary to ask for your approval before reporting those findings?
- What additional genetic diseases can be diagnosed from amniotic fluid besides regular chromosomal and genetic diseases?
- When is the best time for doing the amniocentesis?
- Does the procedure hurt?
- What are the risks of amniocentesis?
- What does the amniocentesis look like?
- What should you pay attention to after the amniocentesis?
- When will I get the results of my amniocentesis?
- What you need to know before coming to the amniocentesis.
Who will benefit from the amniocentesis?
You will benefit from the amniocentesis if the results of your previous screening tests of your current pregnancy indicate a possibly increased risk of chromosomal or genetic disease, or if you, the father of the child or your close relative has a chromosomal or genetic disease.
You can also come to the amniocentesis at your request. No medical indication, referral or doctor's decision is required to go for amniocentesis. The only indication is your own desire - the desire to give birth to a healthy child.
What chromosomal and genetic tests can be carried out with the amniotic fluid taken during amniocentesis?
-
Classical chromosome analysis
- Identifies chromosmal diseases seen under a microscope, including changes in the number of chromosomes (Down syndrome, Edwards syndrome, Patau syndrome) and changes in the number of sex chromosomes (Turner syndrome, Klinefelter syndrom, Jacob's syndrome, Triple X syndrome) and triploidy;
- Unlike Panorama test, this test provides additional information about the structural pathologies of chromosomes.
-
Interphase FISH analysis (iFISH)
- Quick results for discovering the most common trisomies and changes in the number of sex chromosomes within 48 hours;
- In case of a positive rapid test result, it's recommended to confirm the diagnosis with classical karyotyping.
-
Submicroscopic chromosome analysis (CMA analysis)
- Besides chromosomal diseases diagnosed by classical chromosome analysis under a microscope, this modern chromosome analysisanalysis provides information about smaller changes in chromosomes - microdeletions (loss of genetic material) and duplications (addition of genetic material) and copy number variations (CNV) - that cannot be seen under a microscope with the naked eye, but that can cause genetic diseases causing serious invalidities associated with intellectual disability and congenital developmental disorders in children.
- Unlike PanoramaXP test, this test provides information about not only five, but about most of the microdeletions in the child's chromosomes.
-
Gene sequencing panels with the NGS method (NGS analysis)
- Provides information about the smallest units of chromosomes –genes. The analysis of 6,700 genes this test can identify monogenic diseases, including hereditary recessive (both parents pass a defective gene to their child, affects 25% of children) and X-linked diseases (mother is a carrier of the disease, affects her sons). These diseases can often not be discovered before birth and present after birth during the first years of a child's life.
- The purpose of this analysis is to discover definite or possible disease-related genetic variants that cause serious genetic diseases presenting in childhood. With parents' approval, results are given about secondary findings enabling medical intervention that currently includes 73 genes as well*.
- This test examines 25 monogenic diseases assessed in the Vistara test as well as 276 autosomal recessive and X-linked diseases assessed in the Horizon test. It also examines 19 metabolic disorders which newborns are currently being screened for in Estonia.
What do incidental findings during the NGS analysis mean and why it is necessary to ask for your approval before reporting those findings?
The purpose of gene sequencing panels (NGS analysis) is to discover a genetic disease of the fetus that is definitely associated with the child's health and quality of life. In addition to disease-related genetic mutations, there's a list of genetic findings (73 genes) upon which the American College of Medical Genetics (ACMG) has agreed that if the fetus has these findings, parents have to be informed. These are not the kind of genetic findings that would give parents the right to terminate their pregnancy, but knowing them allows you to take action (close monitoring of the child's development, disease prevention, lifestyle changes). The frequency of these incidental findings is 2-3% of examined fetuses. The most common incidental findings are risks of cancer or heart disease. When reporting incidental findings, it's very important to consult a medical geneticist in order to assess the need for parents to take genetic tests.
Reporting incidental findings allows to prevent diseases of the child as well as their parents and to provide more efficient medical care.
Your approval is necessary for describing incidental findings because a positive result may indicate that you are the carrier of this genetic pathology as well and finding this out may be psychologically difficult: you may need to consult a medical geneticist and to further examine your own genes.
-
Incidental findings assessed by gene panel sequencing*
- Familial adenomatous polyposis
- Familial medullary thyroid cancer
- Hereditary breast and/or ovarian cancer
- Hereditary paraganglioma–pheochromocytoma
- syndrome
- Juvenile polyposis syndrome
- Li–Fraumeni syndrome
- Lynch syndrome
- Multiple endocrine neoplasia type 1
- MUTYH-associated polyposis
- Neurofibromatosis type 2
- Peutz–Jeghers syndrome
- PTEN hamartoma tumor syndrome
- Retinoblastoma
- Tuberous sclerosis complex
- von Hippel–Lindau syndrome
- WT1-related Wilms tumor
- Aortopathies
- Arrhythmogenic right ventricular cardiomyopathy
- Catecholaminergic polymorphic ventricular tachycardia
- Dilated cardiomyopathy
- Ehlers–Danlos syndrome, vascular type
- Familial hypercholesterolemia
- Hypertrophic cardiomyopathy
- Long QT syndrome types 1 and 2
- Long QT syndrome
- Biotinidase deficiency
- Fabry disease
- Ornithine transcarbamylase deficiency
- Pompe disease
- Hereditary hemochromatosis
- Hereditary hemorrhagic telangiectasia
- Malignant hyperthermia
- Maturity-onset diabetes of the young (MODY)
- RPE65-related retinopathy
- Wilson disease
Read more:
What additional genetic diseases can be diagnosed from amniotic fluid besides regular chromosomal and genetic diseases?
-
Diagnosing spinal muscular atrophy
- Spinal muscular atrophy or SMA is one of the most common fatal childhood genetic diseases. The incidence rate of SMA is 1/10,000. The incidence rate does not depend on the child's sex.
- SMA is an autosomal recessive genetic disease. For a child to be affected, he/she has to have two defective SMA-causing genes. Healthy parents carry one SMA-causing gene which they both pass to their child who will therefore become ill.
- This disease is characterised by degeneration of spinal nerve cells which causes weakness and atrophy of skeletal muscles.
- The most serious type is SMA type 1 which begins in utero or during the first months of life. The majority of children with this diagnosis die before the age of 2.
- With SMA type 2, the child will develop close to normal until 6 months of age, after that development will slow down and motor skills will start to decline. Parents' first complaint is that the child won't start walking. Some children die in childhood due to respiratory disorders, but the majority will reach adulthood.
- SMA type 3 is the mildest and of slowliest progression of all three SMA types. It begins between the ages of 5-15 and presents as a general muscle weakness and atrophy.
- Although 3 different drugs have been registered in Europe and the USA for the treatment of SMA in recent years, clinical studies regarding their effectiveness and long-term consequences are few. From January 2022, one of the medicines will also be available in Estonia. The earlier the treatment is started, the better the long-term results of the studies.
-
Diagnosing fragile X syndrome
- Fragile X syndrome or FXS is the most common monogenic genetic disease causing intellectual disability. The incidence of FXS is 1:7,000 in boys and 1:11,000 in girls.
- FXS is caused by a defective FMR1 gene on the X chromosome, which is responsible for nerve cell development. Girls have two X chromosomes and if one of them is defective, they will get a milder form of the disease than boys who don't have another healthy X chromosome.
- This disease is characterised by typical appearance and intellectual disability. Boys have more pronounced symptoms than girls.
- 80% of boys with this disease have intellectual disability. Boys with FXS have a large head, a prominent forehead and jaw, large protruding ears, enlarged testicles after puberty, a high-arched palate. Affected boys are more likely to have mitral valve prolapse and enlarged descending aorta. Behavioral disorders are a big problem with boys with FXS: they often experience hyperactivity, restlessness, problems with concentrating, shyness, poor eye contact, autistic behavior, angry outbursts and seizures.
- 35% of girls with this disease have intellectual disability. Girls with FXS have large protruding ears, a long and narrow face, hyperflexible finger joints, flat feet and high birth weight. As for behavioral disorders, they have problems with paying attention, shyness, poor eye contact, restlessness, low self esteem, depression, hyperactivity, nervous movements, inadequate laughing and clapping.
- As of today, there is no cure for FXS, but it is possible to alleviate symptoms. FXS children need a special programme for studying in school as the regular programme is too difficult for them. Heart defects may need surgical correction. Seizures may need anticonvulsant therapy. Antidepressant medications are used for alleviating agressiveness, mood swings and hyperactivity.
When is the best time for doing the amniotic fluid test?
Research has shown that doing amniocentesis before the 16th pregnancy week slightly raises the risk of the fetus developing clubfoot. In order to avoid this risk, no amniotic fluid tests are done before the 16th pregnancy week at the Loote Ultrahelikeskus.
Does the procedure hurt?
During amniocentesis, a thin needle with a sharp tip that punctures abdominal layers with minimal effort and that is designed specially for amniotic fluid tests is used and it causes only minimal pain. The procedure may seem uncomfortable, but most women don't consider it to be more painful than collecting blood, thus previous anesthesia of abdominal layers is not necessary. You may feel light pressure in your abdomen after the procedure, which is normal. The procedure usually lasts for 1-2 minutes.
What are the risks of amniocentesis?
Amniocentesis is a quite common procedure and complications are rare. For most women, the information they get as a result of the examination overweighs the accompanying risk.
The amniocentesis does not harm your baby, but it increases the risk of spontaneous loss of a pregnancy by 0.1%. This is one case per 1000 procedures. The exact reason for miscarriage is unknown. Over 99.9% of pregnancies continue without any problems. The risk of miscarriage is greater with a twin pregnancy than with a single pregnancy. Research shows that the additional miscarriage risk of a twin pregnancy due to amniocentesis is 1%.
Complications most often occur within the first 5 days after the procedure. As the aamniocentesis is guided by an ultrasound, the possibility of injuring the fetus is low.
Sterile technique is used for amniocentesis in order to avoid infections: the abdominal skin is thouroghly washed with antiseptic before the procedure, the abdomen is covered with a sterile sheet, the ultrasound probe is placed into a disposable sterile plastic bag, a sterile gel is used for the ultrasound examination and disposable sterile amniocentesis needles are used for the amniotic fluid test. However, infections that present with fever, uterine contractions and abdominal pain may very rarely occur.
Amniotic fluid is usually a transparent or yellowish odourless fluid. If the fluid is brown or greenish, it's possible to check it for microbes.
Rhesus negative women are at risk of getting the cells of a rhesus positive fetus transmitted into their bloodstream in which case their immune system will start producing antibodies against the fetal rhesus factor. These antibodies may harm the fetus, especially in later pregnancies. If your blood is Rh-negative, you will be given an intramuscular injection that prevents the formation of antibodies immediately after the procedure.
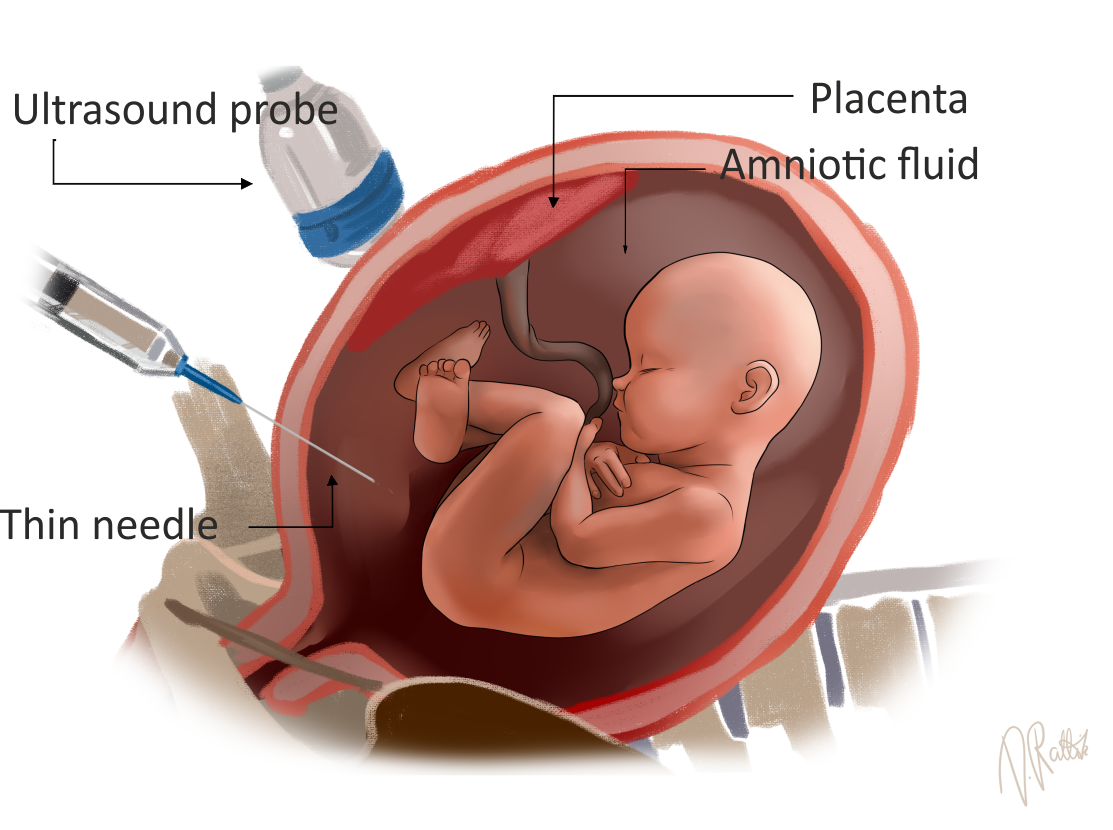
What does the amniocentesis look like?
An ultrasound examination is carried out before the amniocentesis in order to assess the wellbeing of the child in the uterus.
In order to carry out chromosomal and genetic examinations, we need to examine the cells of your future baby. Your fetus is inside the uterus in the amniotic sac filled with amniotic fluid. In amniotic fluid, there are nucleated cells detached from the skin, airways and urinary system of the fetus. In order to examine these cells, 20ml of amniotic fluid is collected with a thin needle through your abdominal wall, guided by an ultrasound image. At this stage of pregnancy, this is an unnecessary amount of amniotic fluid for the fetus that restores within a couple of hours. Amniotic fluid is put into a special germ free tube and sent inside a special container to the labs of the genetic and personal medicine clinic at Tartu University Clinic via courier. Cells from amniotic fluid are placed to grow into a special medium, after which dividing cells can be examined under a microscope or in special automatic genetic analyzers. The needle is removed from the uterine cavity after taking a sample of amniotic fluid and the wellbeing of the child is once again checked by ultrasound examination.
If the fetal membranes have not attached to the uterine wall, the amniotic fluid test won't be carried out and you'll be invited to repeat the procedure after 7 days.
What should you pay attention to after the amniocentesis?
After the procedure you'll be able to continue with your daily activities. You may perceive the puncture site for a couple of following days. If you experience uterine contractions and pain in your lower abdomen, you can orally take paracetamol tablets, if necessary. It's recommended to avoid intense physical activity for the following 24 hours after the procedure.
If you experience strong abdominal or back pain that doesn't respond to analgesics, bleeding, increased watery or abnormal vaginal discharge or a fever higher than 38°C after theamniocentesis, you should immediately see the the gyneacologist on call at the reception of birth givers at the nearest women's clinic. Complications are associated with amniocentesis if they occur within three weeks after the procedure. All complications need hospital treatment. Treatment of complications is usually effective.
When will I get the results of my amniocentesis?
Getting an amniocentesis result depends on the desired chromosomal or genetic disease analysis.
- Results of iFISH analysis 48 hours;
- Results of classical chromsoome analysis 17 days;
- Results of CMA analysis and NGS analysis 35 days;
- Results of spinal muscular atrophy analysis 14 days;
- Results of fragile X syndrome analysis 21 days.
If your results are normal, you will be notified by a call from the genetic laboratory to your given phone number and in a few days, the results will be sent to the Patient Portal and as an encrypted file to your e-mail address. The amniocentesis will inform you about the diseases that are examined. If the results indicate that your fetus has a chromosomal or genetic disease, a medical geneticist will contact you and make an appointment to explain the results and further prognosis of your child's life and health to you. Sometimes it's necessary to examine you and the father of the child for genetic diseases as well.
A missing or extra chromosome, missing or extra genes or pathological changes on the level of a single gene cause alterations in the child's development and as a result, you'll have a sick child. Children with chromosomal and genetic diseases usually have a profound intellectual and physical disability. There is no cure for chromosomal diseases and most of genetic diseases.
According to Estonian laws, termination of pregnancy due to medical reasons is allowed until the pregnancy size of 21 weeks and 6 days.
What you need to know before coming to the amniocentesis.
Before coming to the procedure, we ask you to empty the bladder, remove a belly button piercing (if you have one), not to shave the abdominal area in the morning of the procedure, we ask you to wash yourself throughout the body in the morning of the procedure.
